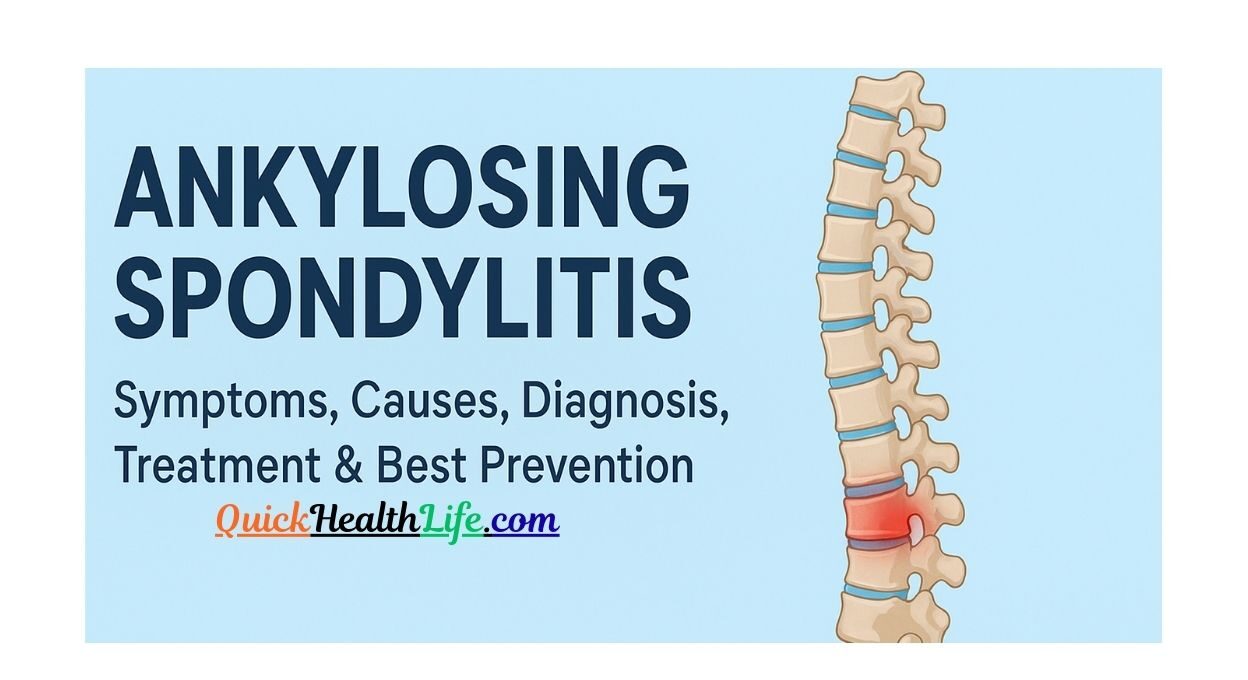
What is Ankylosing Spondylitis?
Ankylosing spondylitis (AS) is a chronic inflammatory disease that mainly affects the spine and sacroiliac joints. Over time, it can cause severe stiffness, reduced flexibility, and in some cases, spinal fusion.This condition usually begins in young adulthood, especially between the ages of 20–40 years, and is more common in men than women. However, women often experience different symptom patterns, making early diagnosis crucial.
Table of Contents
Symptoms of Ankylosing Spondylitis
Recognizing the symptoms early can make a huge difference in managing ankylosing spondylitis effectively. The signs often start slowly and may be mistaken for regular back pain.
Early Stage Symptoms
- Persistent pain and stiffness in the lower back and hips (lasting more than 3 months)
- Pain worse in the morning or after rest
- Fatigue and tiredness due to inflammation
- Mild discomfort in the chest or ribs
Advanced Stage Symptoms
If untreated, the disease can progress, causing:
- Limited spinal flexibility
- Fusion of spinal vertebrae (leading to stooped posture)
- Pain spreading to shoulders, neck, and knees
- Eye inflammation (uveitis) with redness, blurred vision, or pain
- Breathing difficulties if the rib joints become stiff
Ankylosing Spondylitis Symptoms in Females
Women may experience different symptom patterns compared to men:
- More pain in the neck, upper back, and joints instead of the lower back
- Delayed diagnosis because symptoms resemble other conditions like fibromyalgia
- Fatigue and stiffness that worsen with hormonal changes (e.g., after pregnancy
Causes and Risk Factors
The exact cause of ankylosing spondylitis isn’t fully known, but research shows a strong link between genetics and immune system dysfunction.
Role of Genetics (HLA-B27)
- Most patients with ankylosing spondylitis test positive for the HLA-B27 gene.
- However, not everyone with this gene develops the disease.
- It increases the risk by triggering an abnormal immune response that causes inflammation in the joints.
Environmental and Lifestyle Factors
- Family history: If a parent has AS, the risk increases significantly.
- Infections: Some bacterial infections may trigger inflammation in genetically prone individuals.
- Smoking: Worsens symptoms and increases spinal damage.
- Gender & Age: Men are more likely to develop severe symptoms, often starting between ages 20–40.
How is Ankylosing Spondylitis Diagnosed?
Diagnosis can be challenging because early symptoms resemble other back problems. Doctors usually rely on a combination of tests and imaging.
Physical Examination
- Checking posture and spinal flexibility
- Assessing breathing capacity if chest expansion is limited
- Looking for tenderness in the sacroiliac joints
Blood Tests (Including HLA-B27 Test)
- Erythrocyte Sedimentation Rate (ESR) or C-reactive protein (CRP) to check inflammation levels
- HLA-B27 test: Helps identify genetic predisposition
Imaging Tests (X-Ray & MRI)
- X-ray: Detects bone damage or spinal fusion in advanced stages
- MRI: Identifies early inflammation before structural changes appear
ICD-10 Code for Ankylosing Spondylitis: M45
Stages of Ankylosing Spondylitis
The disease progresses through different stages:
| Stage | Key Features | Typical Symptoms |
|---|---|---|
| Stage 1 | Early Inflammation | Mild back pain, morning stiffness |
| Stage 2 | Moderate Symptoms | Reduced flexibility, visible posture issues |
| Stage 3 | Severe Spinal Stiffness | Spinal fusion, difficulty breathing, disability |
Treatment
While ankylosing spondylitis can’t be completely cured, several treatments help manage symptoms, slow disease progression, and improve quality of life.
Medications
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs)
- Examples: Ibuprofen, Naproxen, Indomethacin
- Reduce inflammation, pain, and stiffness
- DMARDs (Disease-Modifying Anti-Rheumatic Drugs)
- Used when peripheral joints (like knees or shoulders) are affected
- Example: Sulfasalazine
- Biologic Agents (TNF & IL-17 Inhibitors)
- Effective in reducing inflammation and preventing joint damage
- Examples: Adalimumab, Etanercept, Secukinumab
- Corticosteroids
- Short-term relief for severe flare-ups
- Not recommended for long-term use
Always consult a rheumatologist before starting or changing medications.
Physical Therapy and Exercise
- Stretching and strengthening exercises keep the spine flexible
- Posture training reduces the risk of spinal deformities
- Swimming and yoga improve joint mobility without extra stress
- Breathing exercises help expand chest capacity
Surgical Options
Surgery is rare but may be required in severe cases:
- Hip replacement if joints are badly damaged
- Corrective spinal surgery in extreme deformity cases
Lifestyle Management and Home Remedies
Apart from medical treatment, lifestyle plays a huge role in managing AS.
Diet and Nutrition
- Anti-inflammatory foods: Fish, olive oil, nuts, leafy greens
- Calcium & Vitamin D: Strengthen bones and reduce risk of osteoporosis
- Avoid processed foods & excess sugar: They worsen inflammation
Daily Exercise and Posture Care
- Maintain straight posture when sitting or standing
- Sleep on a firm mattress to support the spine
- Avoid smoking and excessive alcohol
Tip: Consistency in lifestyle habits works better than temporary changes.
Prevention Tips
Although you can’t fully prevent AS (since genetics play a role), you can reduce complications:
- Get regular check-ups if you have a family history of AS
- Stay physically active daily
- Keep a healthy weight to avoid extra stress on joints
- Avoid smoking and maintain good lung health
- Start treatment early if diagnosed to slow progression
Ankylosing Spondylitis vs Other Conditions
Ankylosing Spondylitis vs Rheumatoid Arthritis
| Feature | Ankylosing Spondylitis | Rheumatoid Arthritis |
|---|---|---|
| Affected Area | Spine & sacroiliac joints | Hands, wrists, knees |
| Onset | Usually before 40 | Any age |
| Genetic Marker | HLA-B27 | RF, Anti-CCP |
| Gender | More common in men | More common in women |
Ankylosing Spondylitis vs Regular Back Pain
- AS pain improves with exercise, worsens with rest
- Regular back pain usually worsens with activity
- Morning stiffness > 30 minutes is common in AS
FAQs on Ankylosing Spondylitis
Q1. Can ankylosing spondylitis be cured?
No, there’s no permanent cure, but treatment can control symptoms and slow progression.
Q2. What is Stage 1 ankylosing spondylitis?
Stage 1 involves mild inflammation and stiffness in the lower back without visible joint damage.
Q3. What is the life expectancy of someone with ankylosing spondylitis?
With proper treatment, life expectancy is almost normal, though severe cases may reduce mobility.
Q4. Is HLA-B27 positive life threatening?
No, being HLA-B27 positive isn’t life-threatening. It just means you have a higher risk of AS.
Q5. How I cured my ankylosing spondylitis – is it possible?
You can’t fully cure AS, but many patients manage it effectively with medication, exercise, and lifestyle changes, leading to a symptom-free life.
Q6. Which test confirms ankylosing spondylitis?
A combination of HLA-B27 blood test, ESR/CRP levels, and MRI/X-ray confirms the diagnosis.