What is Antiphospholipid Syndrome (APS)?
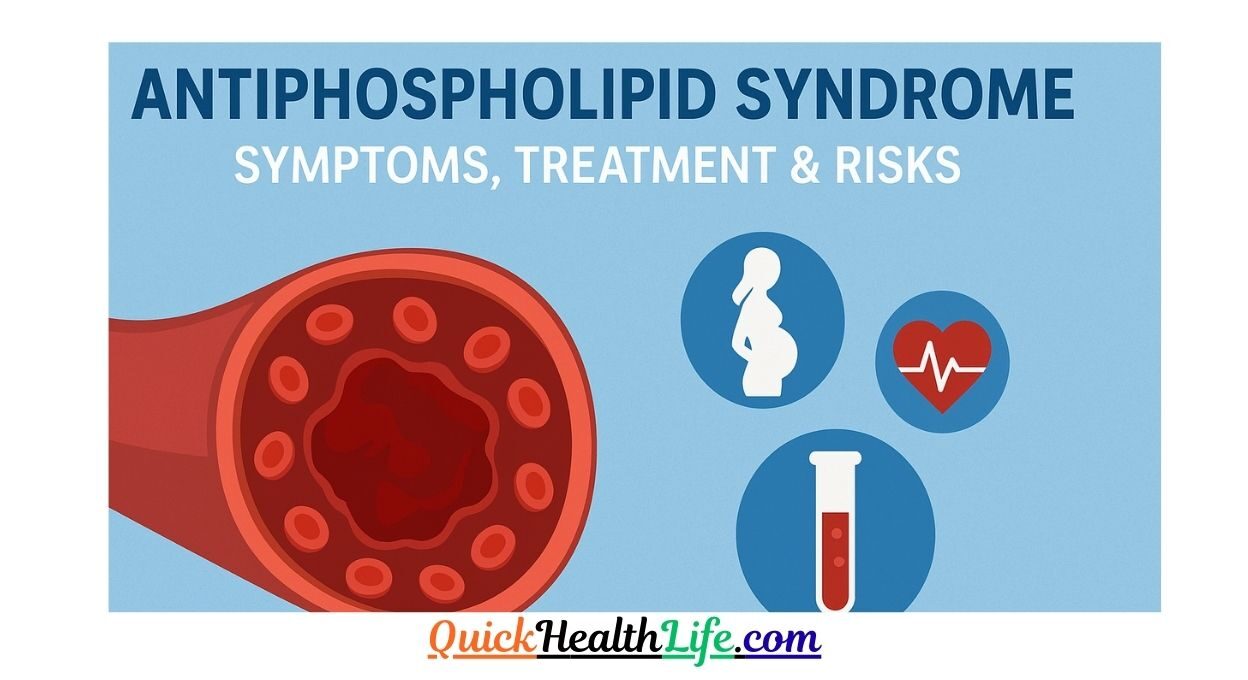
Antiphospholipid syndrome (APS), also known as Hughes syndrome, is an autoimmune disorder where the immune system mistakenly produces antibodies that attack normal proteins in the blood. These abnormal antibodies, called antiphospholipid antibodies (aPL), increase the risk of blood clots (thrombosis) in veins and arteries.
APS affects both men and women but is more common in women of childbearing age. It can occur on its own (primary APS) or alongside another autoimmune condition, like lupus (secondary APS).
This condition is serious because it can lead to deep vein thrombosis (DVT), strokes, heart attacks, recurrent miscarriages, and pregnancy complications. However, with early diagnosis and treatment, most people with APS can live a healthy, long life.
Table of Contents
Symptoms of Antiphospholipid Syndrome
APS symptoms vary depending on which part of the body is affected by blood clots. Some people may not have symptoms until a clot forms, while others may develop recurrent issues.
Common Symptoms in Adults
- Blood clots in veins (DVT) – swelling, redness, and pain, often in the legs
- Blood clots in arteries – leading to stroke, heart attack, or limb pain
- Skin problems – rashes, ulcers, or a lacy purple skin pattern (livedo reticularis)
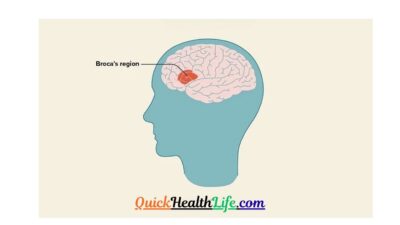
- Neurological symptoms – migraines, seizures, memory issues
- Low platelet count – leading to easy bruising or bleeding
Antiphospholipid Syndrome in Pregnancy
One of the most concerning aspects of APS is its effect on pregnancy. Women with APS are at higher risk of:
- Recurrent miscarriages (especially in the second and third trimesters)
- Preeclampsia (high blood pressure during pregnancy)
- Premature birth
- Stillbirth due to placental complications
Doctors use antiphospholipid syndrome in pregnancy criteria, which include both clinical events (like miscarriages or blood clots) and positive antibody tests, to confirm diagnosis.
Can Antiphospholipid Syndrome Cause Weight Gain?
While APS itself does not directly cause weight gain, certain factors may contribute:
- Medications such as corticosteroids
- Reduced physical activity due to clot-related complications
- Hormonal changes during pregnancy
Maintaining a balanced diet and regular physical activity can help manage weight in APS patients.
Causes and Risk Factors of APS
Antiphospholipid syndrome occurs when the immune system produces antiphospholipid antibodies that mistakenly attack phospholipids (a type of fat) in blood cell membranes. These antibodies interfere with the normal clotting process, making the blood more likely to clot.
What is the Main Cause of Antiphospholipid Syndrome?
The exact cause of APS is still not fully understood. However, medical experts believe it is a combination of genetic and environmental factors. Some possible triggers include:
- Genetic predisposition – a family history of autoimmune diseases increases the risk
- Infections – viral and bacterial infections may trigger antibody production
- Medications – certain drugs like hydralazine or phenytoin can induce antibodies
- Autoimmune disorders – lupus and rheumatoid arthritis are strongly linked with APS
Genetic & Environmental Factors
APS does not always run in families, but people with close relatives who have autoimmune conditions may be more prone to developing it. Environmental triggers, such as infections (hepatitis C, syphilis, HIV) or exposure to certain toxins, may also play a role.
Interestingly, some people may test positive for antiphospholipid antibodies but never develop symptoms. In such cases, lifestyle and other risk factors determine whether APS becomes active.
How Do You Diagnose Antiphospholipid Syndrome?
Diagnosing APS requires a combination of clinical evaluation and laboratory tests. A doctor will look for a history of blood clots, pregnancy complications, or unexplained strokes, and then confirm with blood tests.
Antiphospholipid Syndrome Test & Antibodies
The three main antibodies tested are:
- Lupus anticoagulant (LA)
- Anticardiolipin antibodies (aCL)
- Anti-beta-2 glycoprotein I (aβ2GPI)
For a confirmed diagnosis, the patient must test positive for one or more of these antibodies on two occasions at least 12 weeks apart.
Antiphospholipid Syndrome Rash Pictures & Skin Signs
Skin problems are a key sign of APS. The most common is livedo reticularis, a lace-like purplish rash that appears on the skin due to poor blood flow.
Other skin signs include:
- Painful ulcers on legs or feet
- Necrosis (tissue death) in severe cases
- Small red or purple spots caused by low platelets
(Here, you can insert relevant APS rash images for visual guidance.)
Treatment
APS cannot be cured, but early treatment can prevent serious complications. The main goal is to reduce the risk of blood clots and manage symptoms.
- Blood-thinning medications (anticoagulants)
- Warfarin – commonly prescribed for long-term use
- Heparin – used in pregnancy because it’s safer than warfarin
- Aspirin (low-dose) – reduces clotting risk
- Corticosteroids or immunosuppressants – used rarely in severe APS with autoimmune overlap
Antiphospholipid Syndrome in Pregnancy: Treatment Criteria
Women with APS require special medical attention during pregnancy. Treatment may include:
- Heparin injections (low molecular weight heparin)
- Low-dose aspirin
- Close monitoring with ultrasounds
- Regular blood clotting tests
Following these protocols greatly increases the chances of a safe pregnancy and healthy baby.
Lifestyle Modifications & Foods to Avoid with APS
Lifestyle changes play a big role in managing APS.
What to do:
- Exercise regularly to improve blood flow
- Stop smoking (reduces clotting risk)
- Maintain healthy weight
- Stay hydrated
Foods to avoid with APS:
- Foods high in Vitamin K (spinach, kale, broccoli) if taking warfarin, because they interfere with its effect
- Alcohol – increases bleeding risk
- Processed and fried foods – increase inflammation
Complications of Antiphospholipid Syndrome
If untreated, APS can cause life-threatening complications.
Stroke, Heart Attack & Kidney Damage
- Stroke – blood clots in brain arteries
- Heart attack – blockage of coronary arteries
- Kidney damage – blood clots reduce kidney function, leading to hypertension
Pregnancy-Related Complications
APS is one of the leading causes of recurrent miscarriage. It can also cause:
- Stillbirth
- Placental insufficiency (poor blood supply to baby)
- Intrauterine growth restriction (IUGR)
With proper treatment, most women with APS can successfully carry pregnancies to term.
Life Expectancy with Antiphospholipid Syndrome
One common question is: “What is the life expectancy of someone with antiphospholipid syndrome?”
With proper management, many people with APS live a normal lifespan. However, life expectancy depends on:
- Severity of blood clots
- Presence of other autoimmune diseases (like lupus)
- Early diagnosis and consistent treatment
Prevention & Self-Care Tips
While APS cannot be completely prevented, you can reduce risks with:
- Regular health checkups
- Taking prescribed medications on time
- Avoiding smoking and alcohol
- Staying active
- Following a balanced diet
FAQs About Antiphospholipid Syndrome
1. How do you diagnose antiphospholipid syndrome?
Through blood tests for lupus anticoagulant, anticardiolipin, and anti-beta-2 glycoprotein I antibodies, repeated at least 12 weeks apart.
2. What is the life expectancy of someone with APS?
With treatment, life expectancy can be normal. Risks increase if APS is untreated or associated with lupus.
3. What is the main cause of APS?
The exact cause is unknown, but it involves abnormal immune response producing antiphospholipid antibodies.
4. What foods should you avoid with APS?
Avoid Vitamin K-rich foods if on warfarin, along with alcohol and processed foods.
5. Can antiphospholipid syndrome cause weight gain?
Indirectly, yes. Medications and reduced activity may lead to weight gain, but APS itself doesn’t cause it directly.
6. Is APS a type of lupus?
No, but APS can occur alongside lupus (secondary APS).