Dementia is a hard disease to diagnose for a number of reasons. A new study has found that people who have dementia are, on average, diagnosed 3.5 years after symptoms first appear.This is even longer — an average of 4.1 years after symptoms first show — for people with early onset dementia.
Table of Contents
The 3.5-Year Dementia Diagnostic Gap
A landmark meta-analysis of 30,000+ patients reveals alarming delays:
- Average 3.5 years from first symptoms to formal dementia diagnosis
- Early-onset patients wait 4.1 years – longest diagnostic delays
- Frontotemporal dementia (FTD) faces the longest delays due to atypical symptoms
Why Dementia Diagnosis Takes So Long: 5 Key Barriers
1. Symptom Ambiguity
- Early signs (forgetfulness, mood changes) mimic:
- Normal aging
- Depression
- Thyroid disorders
- Medication side effects
2. Healthcare System Hurdles
| Barrier | Impact |
|---|---|
| Primary care under-training | 40% of early dementia missed in initial visits |
| Specialist shortages | 3-12 month wait for neurologist appointments |
| Reimbursement limitations | Cognitive tests often not covered by insurance |
3. Patient/Family Factors
- Stigma: 65% delay seeking help due to fear/shame
- Misattribution: “Grandpa’s just getting old” mindset
- Socioeconomic gaps: Minority groups face 34% longer delays
4. Disease Complexity
| Dementia Type | Diagnostic Challenge | Avg. Delay |
|---|---|---|
| Alzheimer’s | Gradual onset; overlaps with aging | 3.2 years |
| Frontotemporal | Behavior changes mistaken for mental illness | 4.7 years |
| Lewy Body | Fluctuating symptoms mimic Parkinson’s | 3.8 years |
| Vascular | Stepwise decline attributed to strokes | 3.1 years |
5. Testing Limitations
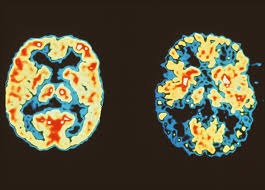
- No single diagnostic test (MRI/CSF/PET scans used in combination)
- Cognitive assessments (e.g., MMSE) have 20-30% false negatives
Early-Onset Dementia: Why Delays Hit Hardest
Patients under 65 face 4.1-year waits because:
- Symptoms attributed to stress (45%) or depression (32%)
- Doctors rarely screen younger patients for dementia
- Atypical presentations:
- Personality changes in FTD
- Vision problems in PCA dementia
- Executive function loss misdiagnosed as ADHD
Closing the Gap: 4 Solutions Backed by Experts
1. Public Awareness Campaigns
- Teach families 7 early red flags:
- Getting lost in familiar places
- Repeated questions/phrases
- Personality shifts (apathy → aggression)
- Trouble handling money/bills
- Forgetting recent conversations
- Misplacing items oddly (keys in fridge)
- New language struggles
2. Primary Care Upgrades
- Mandatory 5-minute cognitive screens at Medicare physicals
- Validated tools: Mini-Cog, MoCA, GPCOG
- Clear referral pathways to specialists
3. Specialist Access Expansion
| Innovation | Impact |
|---|---|
| Tele-neurology consults | 65% faster access in rural areas |
| “Dementia Diagnostic Centers” | One-stop testing (MRI + labs + neuropsych) |
| Pharmacist cognitive screens | Community-based early detection |
4. Biomarker Breakthroughs
- Blood tests for p-tau217 (90% accurate for Alzheimer’s)
- AI analysis of speech patterns/writing samples
- Retinal scans detecting amyloid plaques
FAQs About Dementia
Q1: Why can’t we diagnose dementia faster?
A: No definitive test + symptoms overlap with 20+ conditions. Diagnosis requires ruling out mimics.
Q2: What’s the #1 reason families delay seeking help?
A: Stigma – 68% fear “dementia” label more than cancer (Per Alzheimer’s Society).
Q3: Can you diagnose dementia in one visit?
A: No – requires:
- Cognitive testing
- Blood work (B12/thyroid)
- Brain imaging
- Symptom tracking over months
Q4: Who diagnoses dementia fastest?
A: Patients with:
- Strong family advocacy (cuts 1.8 years off delay)
- Academic medical center access
- ApoE4 genetic risk (qualifies for early testing)
Q5: Does early diagnosis improve outcomes?
A: Yes – allows:
- Medication to slow decline (donepezil, memantine)
- Safety planning (driving, finances)
- Clinical trial access
Q6: How much does diagnosis cost?
A: $1,200-$5,000 (MRI + neuropsych eval + specialist visits). Medicare covers 80%.
Q7: What questions should families ask doctors?
A:
- “Could this be something besides dementia?”
- “When should we see a specialist?”
- “What tests are needed to rule out mimics?”
Q8: Are online dementia tests accurate?
A: No – 89% of direct-to-consumer tests give false positives/negatives (JAMA study).
Q9: Can you have dementia with a normal MRI?
A: Yes – especially in frontotemporal dementia. Clinical assessment is key.
Q10: What policy changes would help?
A:
- Medicare coverage for annual cognitive screens
- Loan forgiveness for dementia specialists
- Mandatory medical training in dementia detection
Global Impact: Dementia by the Numbers
| Statistic | Value | Source |
|---|---|---|
| Global dementia cases (2024) | 57+ million | WHO |
| Annual new cases | 9.9 million | Lancet Neurology |
| Diagnosis cost to families | $8,100 pre-diagnosis | Alzheimer’s Association |
| Years lived with disability | 28.8 million | Global Burden of Disease |
4 Actions to Speed Up Your Diagnosis
- Track symptoms in a journal (include dates/examples)
- Request a Mini-Cog test at your next physical
- Seek specialists if:
- Symptoms worsen over 6 months
- Multiple cognitive domains affected
- Explore clinical trials at Alzheimers.gov