Inflammatory Bowel Disease (IBD) — primarily consisting of ulcerative colitis (UC) and Crohn’s disease (CD) — affects millions worldwide. While genetics and immune dysfunction play a significant role, emerging research reveals that diet and lifestyle choices also contribute to the risk and severity of IBD. This article breaks down the connection between food and IBD, backed by the latest research, structured data, FAQs, and practical tips.
Table of Contents
What is Inflammatory Bowel Disease (IBD)?
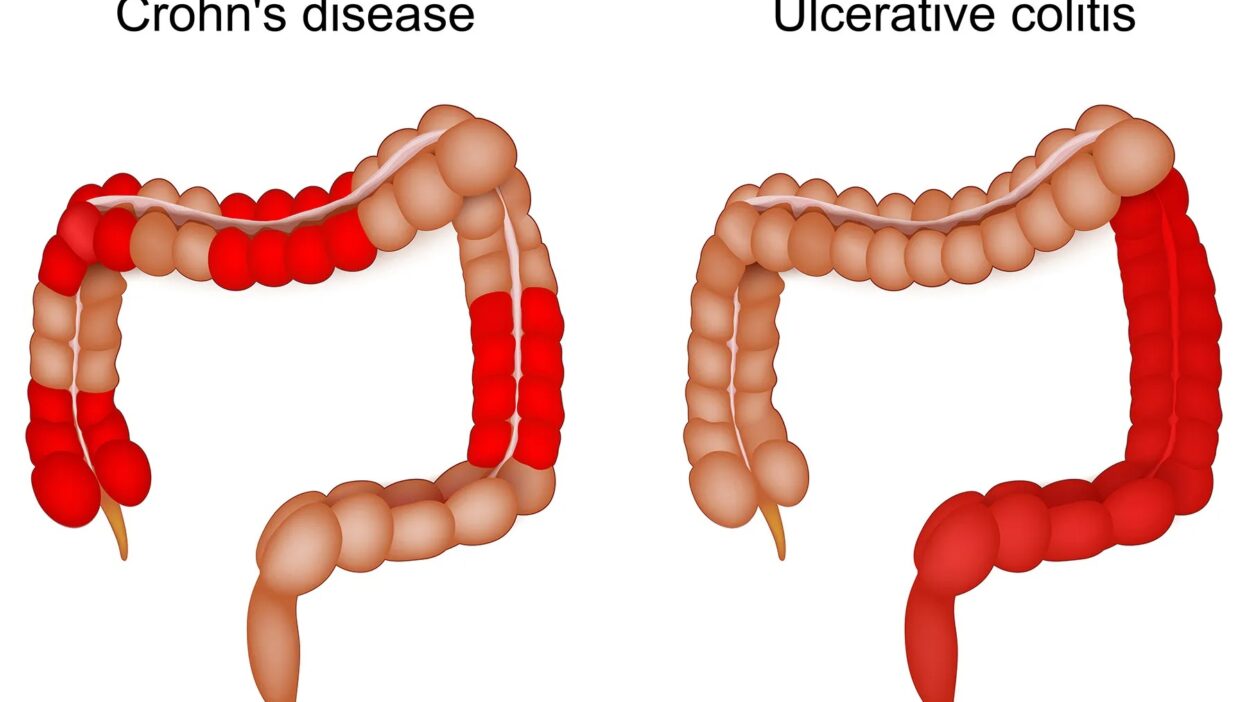
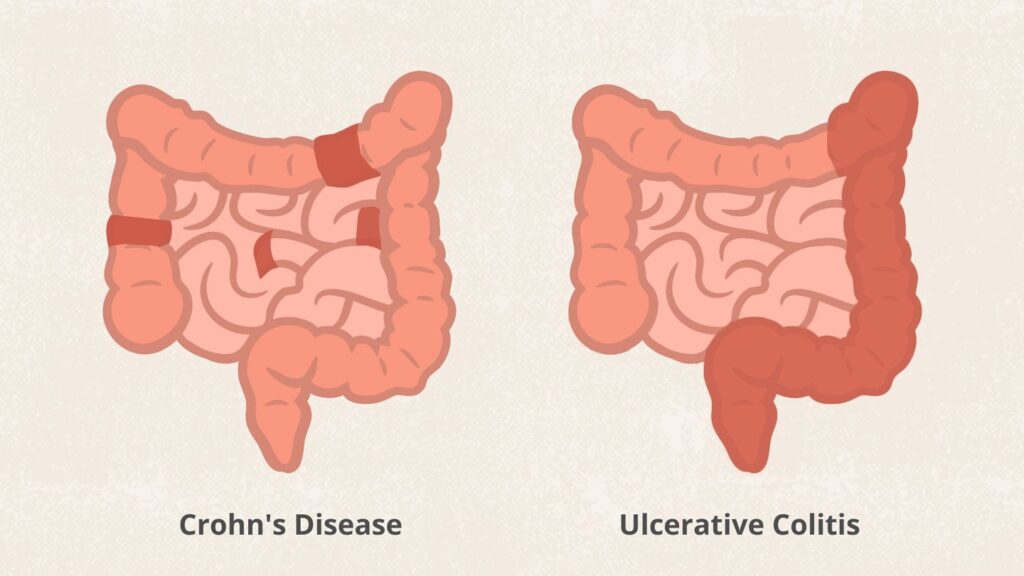
Inflammatory Bowel Disease (IBD) is a chronic condition causing inflammation in the digestive tract. The two main types are:
- Ulcerative Colitis (UC): Affects only the colon and rectum.
- Crohn’s Disease: Can affect any part of the GI tract, from mouth to anus.
Unlike temporary stomach bugs, IBD involves long-term inflammation, leading to ulcers, pain, and severe digestive issues. While there’s no cure, the right treatment can control symptoms and even lead to remission.
Ulcerative Colitis vs. Crohn’s Disease: Key Differences
| Feature | Ulcerative Colitis | Crohn’s Disease |
|---|---|---|
| Location | Only colon & rectum | Any part of GI tract |
| Inflammation Depth | Inner lining only | All layers of bowel wall |
| Pattern | Continuous | Patchy (“skip lesions”) |
| Common Symptoms | Bloody diarrhea, urgency | Abdominal pain, weight loss |
| Smoking Effect | May reduce risk | Worsens disease |
IBD Causes & Risk Factors
The exact cause is unknown, but these factors play a role:
✅ Genetics – Family history increases risk.
✅ Western Diet – High in processed foods, low in fiber.
✅ Smoking – Increases Crohn’s risk but may protect against UC.
✅ Gut Microbiome Imbalance – Bad bacteria overpower good ones.
✅ Autoimmune Response – Immune system attacks the gut.
✅ Ultra-Processed Foods – Strongly linked to Crohn’s (2024 study).
Common IBD Symptoms
- Abdominal pain & cramping
- Persistent diarrhea (sometimes bloody)
- Urgent bowel movements
- Unintended weight loss
- Fatigue & low energy
- Fever & night sweats
- Joint pain & swelling
How is IBD Diagnosed?
Doctors use:
🔹 Colonoscopy (with biopsy) – Gold standard.
🔹 Stool tests (calprotectin, infections).
🔹 Blood tests (CRP, ESR, anemia).
🔹 CT/MRI enterography (for Crohn’s).
Best Treatments for IBD
1. Medications
- Aminosalicylates (5-ASA)
- Corticosteroids – Short-term flare control.
- Immunomodulators – Long-term immune.
- Biologics (Anti-TNF, IL-12/23 inhibitors) – Game-changers for moderate-severe IBD.
- JAK Inhibitors – New oral option (e.g., Rinvoq).
2. Surgery
- Colectomy (for severe UC).
- Bowel resection (for Crohn’s strictures).
3. Diet & Lifestyle
✔ Mediterranean diet (best for Crohn’s).
✔ Low-FODMAP during flares.
✔ Probiotics (VSL#3, Saccharomyces boulardii).
✔ Stress management (yoga, meditation).
Foods to Eat & Avoid with IBD
| Eat More | Avoid |
|---|---|
| Cooked veggies | Spicy foods |
| Lean proteins (fish, chicken) | Fried & greasy foods |
| Bananas, applesauce | Dairy (if intolerant) |
| Fermented foods (yogurt, kefir) | Processed meats |
| Omega-3s (salmon, flaxseeds) | Alcohol & soda |
FAQs About IBD
1. What triggers an IBD flare-up?
Common triggers:
- Stress
- Infections
- NSAIDs (ibuprofen, aspirin)
- Processed foods
- Smoking (for Crohn’s)
2. Can diet cure IBD?
No, but it can reduce flares and inflammation. The Mediterranean diet is best for Crohn’s, while low-residue diets help during UC flares.
3. Is IBD the same as IBS?
No! IBD = inflammation (UC, Crohn’s). IBS = no inflammation (functional disorder).
4. When is surgery needed for UC?
If:
- Medications fail
- Toxic megacolon develops
- Cancer risk is high
5. Can probiotics help IBD?
Some strains (like VSL#3) may reduce inflammation, but always consult a doctor first.